Porphyromonas gingivalis (Pg) is a keystone pathogen with strong links to severe periodontal disease (PD).
Found deep in the tooth root pocket, together with other bacteria, Pg is believed to disrupt the homeostasis of the oral microbiome, triggering chronic inflammation.
Patient impact of severe periodontal disease
Severe PD is a debilitating gum disease that affects people across all income groups, with its prevalence being highest in smokers and diabetics.
Those in lower socioeconomic demographics are more likely to experience severe symptoms due to a lack of access to appropriate and affordable care.
The disease damages the periodontal soft tissue and alveolar bone that supports the teeth, which can ultimately lead to affected teeth falling out.
Severe PD causes physical pain and is also associated with an increased risk of anxiety disorder (by 35%) and depression (by 70%).

The World Health Organisation estimates there are more than one billion cases of severe periodontal disease worldwide (19% of all adults) with periodontitis inflicting a significant economic burden with direct and indirect treatment costs of $349Bn estimated in the USA alone.

Current treatments
Current treatments, such as scaling and root planning, are painful, expensive and not available to all patients.
There are no approved medical therapies, other than topical antibiotics, to reduce the incidence of Pg-related PD.
The role of Porphyromonas gingivalis in severe periodontal disease.
Porphyromonas gingivalis (Pg) is a keystone pathogen with strong links to severe periodontal disease. Found deep in the tooth root pocket, together with other bacteria, Pg is believed to disrupt the homeostasis of the oral microbiome, triggering chronic inflammation.
Pathogenic Pg deep in the pocket multiple and release microbial toxins that cause gum inflammation and bleeding. The blood acts as a food source for Pg (and other bacteria), helping them to multiply. Pg microbial toxins make it difficult for your immune system to control the growth of Pg.
The inflammation caused by Pg and the microbial toxins it secretes, eventually destroys the tooth ligaments and the bone of the tooth socket unless successfully treated.
Chronic diseases linked with Porphyromonas gingivalis
Pg is not only associated with severe PD. There is a growing body of research identifying potential links between Pg and other diseases including arthritis, cardio-vascular diseases, certain cancers, and Alzheimer’s disease.
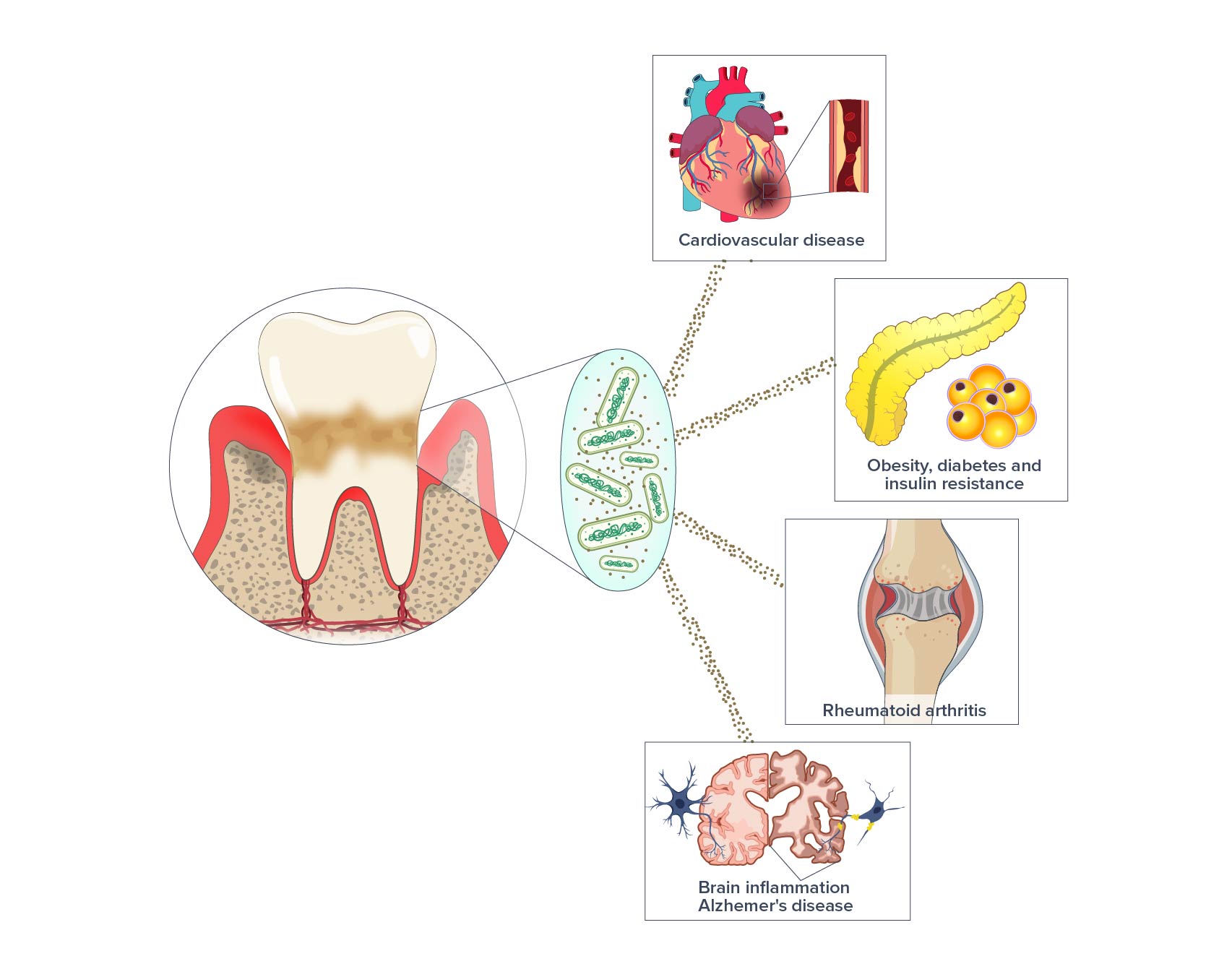
Alzheimer’s disease
P. gingivalis releases toxins called virulence factors. Research has found these virulence factors in the brains of patients with Alzheimer’s, with their levels correlating to the level of Alzheimer’s disease pathology.
In a recent clinical study, a drug targeting the virulence factors resulted in a slowing down of the cognitive decline in Alzheimer’s disease patients with oral Pg.
Diabetes
P. gingivalis has long been associated as a risk factor with diabetes. The virulence factors produced by Pg contribute to insulin resistance by disrupting insulin signaling pathways.
Heart disease
P. gingivalis, has been found in lesions of the cardiovascular system and shown to promote the development of atherosclerosis and disrupt endothelial integrity.